The hip is a ball-and-socket joint made up of the femur (ball) and acetabulum (socket). Although the deep socket makes the hip inherently stable, it is further reinforced by a lining (capsule) and a ring of supporting fibrocartilage (labrum). In a normal hip joint, all of these structures function together to allow for smooth movement of the joint without conflict or instability.
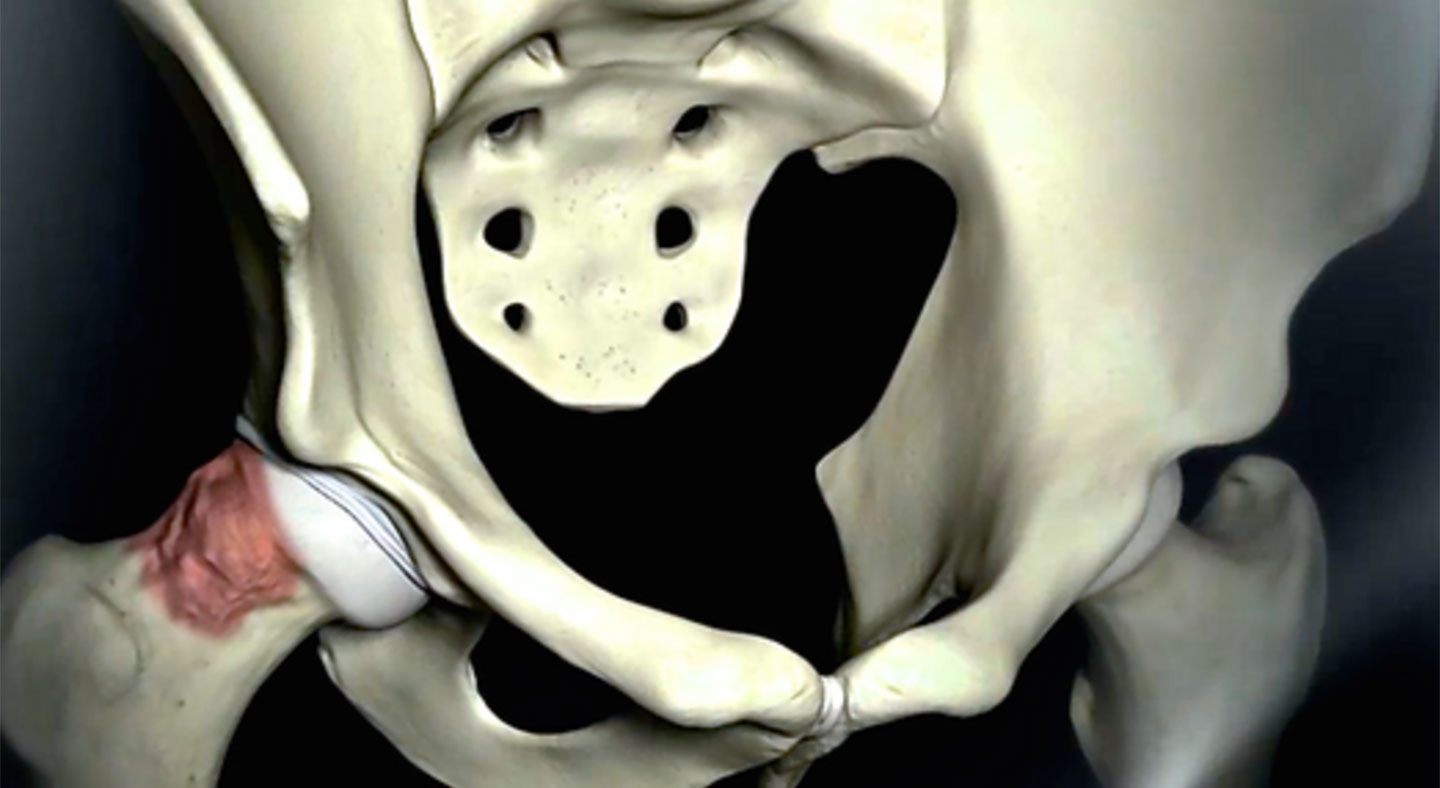
The term femoroacetabular impingement (or FAI) refers to a condition in which movement of the hip joint is restricted due to abnormal bony contact between the ball and acetabulum socket. A common cause of FAI is a developmental abnormality of the ball resulting in bony overgrowth (cam lesion), which abuts against the rim of the socket during deep hip flexion and internal rotation. Alternatively, FAI may come about due to an excessively deep or abnormally oriented socket (pincer lesion) with a similar painful restriction in motion. Sometimes, the bony abnormality is quite subtle and impingement is due to the high demands placed on the hip (ballet, hockey, soccer, etc.). Over time, repetitive impingement can cause tearing of the labrum, surface cartilage damage, and early arthritis.
Patients with FAI typically present with activity related groin pain and/or mechanical symptoms such as painful clicking and catching deep in the hip. Over time, the pain may become constant and significantly limit the patient’s ability to participate in both recreational activities and activities of daily living, or sit for prolonged periods of time. It is also common for these symptoms to affect activities of daily living and intercourse.
The first line of treatment is conservative management, consisting of activity modification to avoid positions of impingement, physical therapy to strengthen the surrounding musculature, and various injections to reduce inflammation and provide temporary relief (we strongly discourage steroid injections as they have the propensity to damage joint’s cartilage). When these measures fail to provide adequate relief of symptoms, the next step is to surgically correct the underlying structural abnormality and cause of symptoms.
Surgery for FAI has evolved dramatically over the past 15 years, from open surgical dislocation to minimally invasive hip arthroscopy with ever growing specialized equipment and techniques. The goal of surgery is to repair the torn labrum with the use of anchors, reshape the ball and socket by removing excess bone to resolve the impingement conflict, and address any surface cartilage damage by cartilage regeneration techniques. Ideally, surgery for impingement should be performed prior to the onset of significant surface cartilage damage, as this may be irreversible and, when present, may result in inferior outcomes.
For cam-FAI and pincer-FAI, hip arthroscopy alone is sufficient to completely address all injured structures and reconstitute a normal anatomy and hip biomechanics. Rarely, another developmental parameter (rotational alignment of the femur – or femoral torsion) may contribute to and exacerbate the impingement in the hip, requiring additional treatment. When the femur bone is mal-rotated (femoral retrotorsion), there is excessive hip external rotation and limited hip internal rotation. This shift in the hip’s rotation arc further compounds the negative effects of cam- or pincer-FAI and may require a realignment procedure (derotational femoral osteotomy – or DFO) to restore normal femoral rotational alignment. Although a DFO is performed in a minimally invasive way, the combined surgery results in a more prolonged recovery.
Whether hip arthroscopy is a worthwhile option for a patient depends on a number of factors, including:
In general, the outcomes of hip arthroscopy are best in patients < 50 years of age (and optimally, < 40) with focal or discrete structural damage and minimal arthritis. The team will guide you through the various considerations in helping you decide whether hip arthroscopy is right for you.
However we have treated successfully patients 55-60 years old for both FAI and dysplasia, as long as their joint was biologically “young”. We like to say that we determine the viability of the joint for Preservation procedure by the “biological age” of the joint, rather than by the “chronological age” of the patient.
Choosing the treatment option that is right for you involves careful consideration of your diagnosis, duration and severity of symptoms, desired level of activity, as well as social and financial elements. You are not alone in this process.
As you research your condition, please write down all of your questions and bring them with you to your next appointment. Dr. Mei-Dan, Dr. Lee and the team at CU Sports Medicine Hip Clinic will take time to address all of your concerns, until you are completely satisfied with your treatment plan.