Hip replacement surgery is for when hip preservation surgery is no longer, or not a good option for hip arthritis, hip dysplasia, or other end stage hip disease. It is performed either under general anesthesia or sedation with spinal analgesia depending on the health and safety of the patient first and foremost.
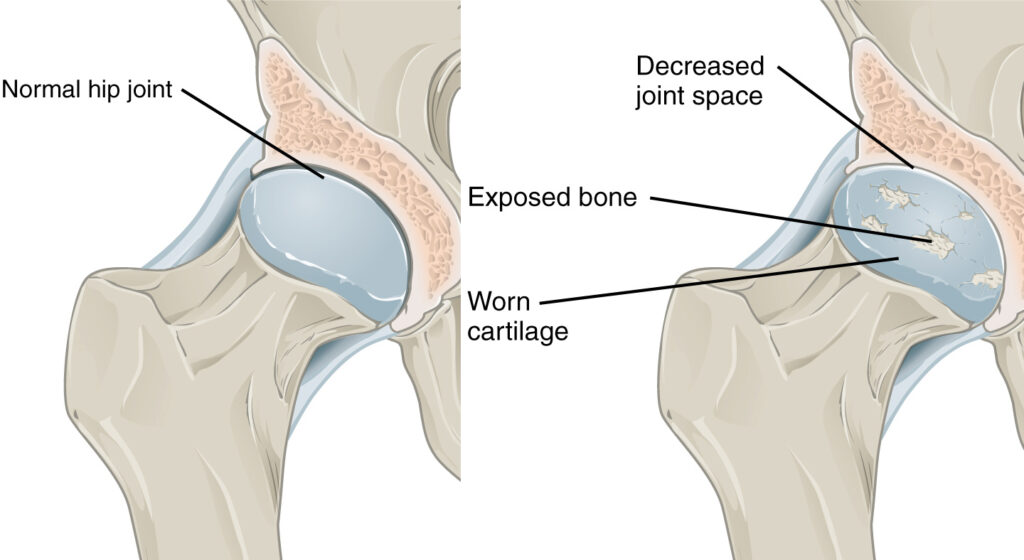
The hip is a ball and socket joint lined with articular cartilage, which is a smooth, minimal friction interface which allows for a wide arc of motion of the lower extremity, and stable high impact weight bearing. When the cartilage is lost as a result of progressive arthritis, the hip joint degenerates, causing both the femoral head (ball) and the acetabulum (socket) to change shape in such a way that leads to loss of motion, pain with activity, and pain at rest. When hip preservation, nonoperative interventions such as injections, lifestyle modifications, and other conservative treatment strategies no longer help, hip replacement surgery offers long term relief.
Hip replacement surgery will remove the arthritic joint in entirety with specialized instruments and replaces the native, diseased hip joint with new prosthetics which will either integrate into the native bone, or will be fixed with bone cement if the bone is weak or brittle. Acetabular implants (cup) are most frequently made out of a porous metal (in the United States) which allows the bone to grow into it ideally for permanent fixation. This is then lined with an ultra high molecular weight crosslinked polyethylene (surgical grade plastic) liner. The femoral component is typically a wedge, tapered design which is seated into the top of the femur after the head and part of the neck has been removed, and sized to fit the patient’s native anatomy if appropriate.


Sometimes cement is necessary to fix the femoral component to the femur if the bone is at risk of fracture during the surgery. For patients with soft or osteoporotic bone, cement fixation is often a safer option than “press fit” implants.
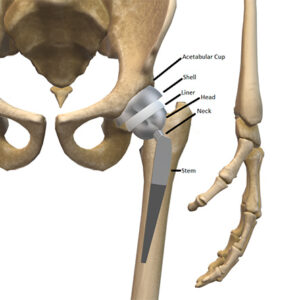 The native head (ball) is replaced with either a metal or ceramic head, which sits perfectly in the plastic liner. The goal of this is to provide long lasting improved function, and pain relief in patients with end stage hip disease.
The native head (ball) is replaced with either a metal or ceramic head, which sits perfectly in the plastic liner. The goal of this is to provide long lasting improved function, and pain relief in patients with end stage hip disease.
Hip replacement implants come from different manufacturers, and have different designs similar to makes and models of cars. Although hip replacement surgery is one of the most common elective procedures performed, it is not a one size fits all surgery. Therefore, different patients will require different “makes and models” of their implants depending on their anatomy (underlying hip dysplasia, excessive femoral antetorsion to name a few), bone strength, metal sensitivity, spine disease, dislocation risk(s)). Your surgeon will pick the implant(s) based off of these considerations, and preference for implant system(s).
Your surgeon may use a robot to assist with parts of the surgery. For hip replacement surgery, the robot is used for precise bone resection usually on the socket side, and for accurate placement of the acetabular component (socket). The use of a robot requires advanced imaging such as a CT scan done at least two weeks prior to the scheduled surgery. This allows the surgeon to create a personalized plan for your surgery and template the position of your implants based on your own anatomy before you even go to the operating room! You can think of the robot as a stable “extra arm” that the surgeon uses to make the surgery easier, and more accurate. Using the robot can also decrease the number of x rays needed to ensure precise placement of components.
Minimally Invasive Surgery
Although minimally invasive joint replacement surgery sounds like less surgery, it is actually the same amount of surgery through a smaller incision. This is not always an appropriate option for everyone as the primary objective is to perform an effective surgery safely and efficiently. Although there are benefits to minimally invasive surgeries such as smaller scars, less pain early on, and possibly some muscle sparing, these things are not as important as making sure the joint replacement goes in correctly. The biggest obstacle to a minimally invasive approach is body size, weight and habitus. If minimally invasive surgery does not work for your body type, the surgeon will choose the safest incision for your body to ensure a successful joint replacement surgery.
Direct Superior Approach
When this is an option for your body type, the direct superior approach is a muscle splitting approach, which creates a mobile window to the hip joint. The proposed benefits of this approach are decreased blood loss, faster recovery, sparing of a structure called the Iliotibial (IT) band, and sometimes the piriformis muscle. This is proposed to increase soft tissue stability following joint replacement surgery, and therefore helps mitigate prosthetic dislocation risk. No approach has a zero dislocation risk, and the direct superior approach is one of many. It does create a smaller incisional scar, which can easily be hidden with a conservative bikini bottom.
If you have had a steroid injection into your hip or knee joint in the last 3 months, you will have to wait until at least 3 months following the injection for surgery. Steroid injections within a 3 month period prior to joint replacement surgery puts you at higher risk for prosthetic joint infection.
Dr. Lee adheres to these nationally and association recommended clinical practice guidelines recommended by the American Association of Hip and Knee Surgeons (AAHKS):
At discharge you will receive a post op folder with instructions on how to care for your dressings and when you may bath or shower. We ask that you do not remove your dressings unless they are saturated or leaking. If you are unsure, please review our instructional videos and call if needed. The post op folder will also include your medication instructions, a Persons With Disabilities parking privileges application and your hip arthroscopy photos. There is a pain/medication tracking sheet you will be asked to fill out and bring to the first post op appointment. A hip preservation team contact list will also be provided; use this to reach out with urgent matters.